Jaundice is defined as the yellow discoloration of the skin, earliest sign is slceral icterus (yellow discoloration of the sclera) that can be from overproduction or underclearance of bilirubin.
- Due to increase serum bilirubin (total) >2.5mg/dL, arising from disturbed BR metabolism
- Direct bilirubin (Conjugated bilirubin) – soluble in water and can be excreted in the urine or converted to urobilinogen by GI bacteria esp in colon. (dark urine only seen with direct Br)
- Indirect bilirubin (unconjugated bilirubin) – non-soluble in blood hence carried by albumin and hence never seen in urine even if high. Toxic to CNS can pass BBB (blood brain barrier).
- 3 Major causes (in a nutshell): Hemolysis, Liver disease, Biliary obstruction.
Normal BR metabolism from RBC
Table of Contents
- RBC consumed by Mphage in the RES, protopropyrin converted to UBR and carried by albumin to liver for conjugation to form CBR. Enzyme in the liver called UGT in hepatocytes conjugates the BR which is transported to bile canaliculi to form part of bile and store in the gall bladder.
- Insoluble UBR is held by the albumin floating in the serum. It does not get excreted in the kidney as it is not soluble.
- Bile is released into the small intestine to aid in digestion (especially fat)
- Intestine flora converts CBR to urobilinogen and later oxidized to Urobilin=Sterobilin(brown) to make the stool brown.
- Some of urobilinogen is absorbed to blood, some go back to liver, some goes to kidney, and converted to a yellow pigment (urobilin) in urine at the kidney,
Terminology and Presentation of Cholestasis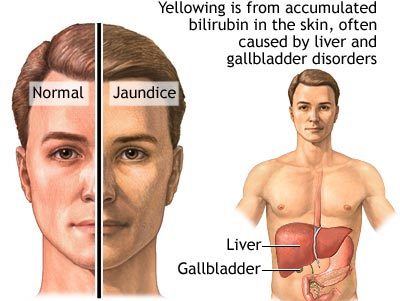
- Cholestasis: blockage of bile flow (whether intrahepatic or extrahepatic) and hence lead to an elevation of conjugated bilirubin in blood.
- Clinical findings of Cholestasis: jaundice, dark urine, pale stool, pruritis (bile salt deposit in skin)
- Labs in cholestasis: elevated alkaline phosphatase (ALKP), elevated cholesterol (due to impaired excretion) skin xanthoma.
- Malabsorption of fat and fat soluble vitamins (steatorrhea)
Etiology and Association:
- Unconjugated Bilirubinemia (Increase UBR)
- Increase RBC turnover
- Physiological jaundice (newborn babies) coz liver not well develop yet
- Reduce uptake from liver Hereditary – (Gilbert and Crigler-Najjar Syndrome)
- Hepatitis, Cirrhosis hence interfere with conjugation of BR
- Drugs (sulfonamide, PCN, rifampin, radiocontrast)
- Conjugated Bilirubinemia (Increased CBR)
- Liver Disease
- Cirrhosis (late stage = problem with excretion and conjugation)
- Hepatitis
- Decrease intrahepatic excretion
- Liver disease (cirrhosis, hepatitis)
- Inherited disorder (Dubin-Johnson = canaliculi transport protein defect); (Rotor Syndrome-same but no darkening/blackening of liver)
- Primary/Secondary Biliary Cirrhosis, PSC
- Drug induced (OCP)
- Extrahepatic biliary obstruction
- Gall stone, Tumor (pancreatic, liver, cholangiocarcinoma),
- Stricture –Primary sclerosing cholangitis, biliary atresia
- Parasite (Liver Fluke worm)
- Liver Disease
Pre Hepatic:
- Increased unconjugated bilirubin
- Overproduction of BR (hemolysis in hemolytic anemia)
- Overproduction from ineffective EPoesis hence RBC die
Intra-Hepatic:
- Defective BR Uptake – Drugs (OCP, ↑Estrogen),Diffuse liver disease (hepatitis, cirrhosis)
- Conjugation – Enzyme Deficiency, Cirrhosis, hepatitis, tumor
- Excretion – Impaired excretion of transport into bile duct (Bile duct damage/transporter), 1o Biliary Sclerosis
Post Hepatic:
- Biliary obstruction (extrahepatic biliary atresia, Gall stones (CBD obstruction), Carcinoma of pancreas head, Primary Sclerosing Cholangitis)
Diagnosis
- Measure serum levels of bilirubin
- Follow the chart is next page
Treatment and Management
The treatment and management of jaundice depend on the cause. Read the different types of jaundice for the treatment and management.