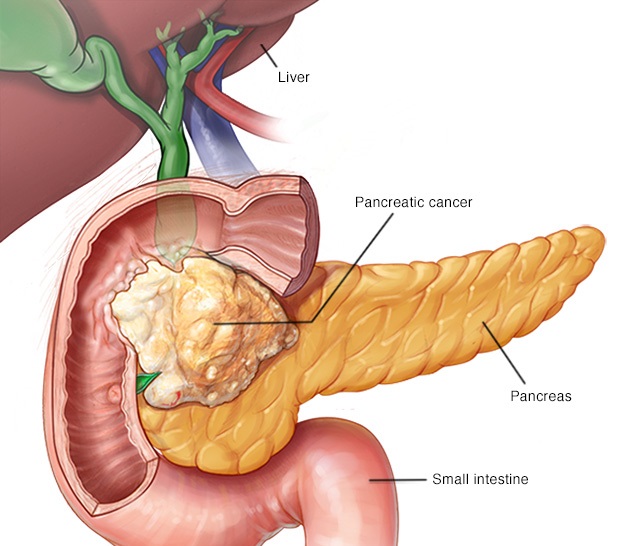
Pancreatic tumors can be classified into four categories: We will focus on adenocarcinoma here since it is the type of cancer found in 95% of diagnosed pancreatic cancer.
- Epithelial: Ductal Epithelium (adenocarcinoma), Cystic neoplasm (Serous/Mucinous: IPMN, MCN)
- Neuroendocrine tumor (PNET): Can be Functional or Non-functional (see later)
- Exocrine tumor: Acinar Cell Carcinoma
- Mesenchymal tumor (rare)
Pancreatic adenocarcinoma is the the scariest cancer that can affect humans. It is no coincidence that they are referred to as the “king of cancer”. The prognosis for pancreatic adenocarcinoma arising from the pancreatic duct epithelium is very poor and most cases are metastatic at the time of diagnosis.
Etiology and Risk factors of Pancreatic Adenocarcinoma
Table of Contents
- Pancreatic adenocarcinoma are most commonly seen in elderly around 70 years old.
- Risk factors for pancreatic adenocarcinoma include: Smoking is the most important risk factor) and have been shown in many studies. Other associations like chronic pancreatitis, Diabetes mellitus type 1, Fatty Diet, Alcohol intake are all inconsistent risk factors.
- Genetics have shown some association between patient with BRCA/Peutz-jegher syndrome and link to pancreatic adenocarcinoma.
Symptoms and Clinical Presentation
- Epigastric pain that radiate to the back and weight loss are seen in 90% of patients.
- Jaundice and icterus (if tumor block the biliary tree esp head of pancreas) ie blockage of intrapancreatic common bile duct (CBD) which is a sign of advanced disease.
- Recent onset of diabetes mellitus and glucose intolerance that is mild.
- Migratory Thrombophlebitis (MT) = Trousseau Syndrome of Malignancy (10% have this symptom)Spontaneous venous thrombosis which may resolve and recur due to release of PAF and pro-coagulatory factors from some tumors (Pancreatic adenocarcinom is common)
- MT associated with visceral malignancy, most often occurs in the superficial vein of the upper and lower extremities
- Tumor Blockage: Signs of Chronic Pancreatitis and Obstructive Jaundice
- Steatorrhea (enzyme), lack of absorption of Vitamin ADEK, B12 deficiency (B12 because no enzyme to cleave R binder)
- Pale stool (tumor block bile release into duodenum)
- Palpable Non-tender gall bladder (when tumor spread and also blocks biliary tree in a short period of time hence back up pressure cause distension of gall bladder), usually accompanied with jaundice – “Courvoisier’s law” which states that in the presence of an enlarged gallbladder which is nontender and accompanied with mild jaundice, the cause is unlikely to be gallstones instead likely to malignancy like (Gall bladder cancer, Pancreatic cancer) – note for Gall stones (right upper quad abdomen pain that radiates to right shoulder – Tender)
- Differential diagnosis: Gallstones vs Pancreatic Cancer Metastasis: Gallstones usually non-palpable This observation occurs because gallstones are formed over an extended period of time, resulting in a shrunken, fibrotic gall bladder which does not distend easily. This shrunken gallbladder is less likely to be palpable on exam
- Secondary Diabetes (if tumor occur at body or tail)
Lab Markers
- Serum marker CA19-9, CEA
- SiADH (paraneoplastic syndrome)
- These markers are not meant for diagnosis but for following post treatment prognosis
Diagnosis
- If jaundice present – US abdomen (to rule out biliary tract obstruction) – poor visualized pancreatitis or pancreatic necrosis due to overlying bowel gas from ileus. US is also not good for tumors < 3 cm visualization.
- If jaundice not present – CT scan abdomen can diagnose pancreatitis and also pancreatic cancer and the metastatic status (staging)
- ERCP most sensitive
- US: intra and extra hepatic biliary tract dilation from tumor head blockage (elevated Alkaline phosphatase)
- X ray: double duct sign
- Tumor desmoplasia (stromal fibrosis) and perineural invasion (cancer spread surrounding the nerve) are common
- Most of the time the cancer occur at the head (75%), Body (20%) , Tail (10%)
Progression/Course of Disease/Complications
- Very poor prognosis involve a massive procedure called Whipple Procedure.
- Diabetes Mellitus (cannot make Insulin)
- Blockage of Common Bile duct (head of pancreas)
- Portal vein thrombosis
Treatment and Management:
- Surgical resection – whipple procedure is the only hope for cure (only 10% resectable)
- ERCP/PTC with stent placement to alleviate obstruction for palliation.