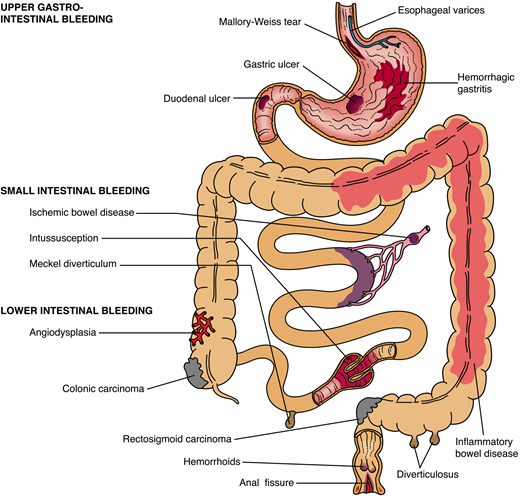
Bleeding in the any part of the gastrointestinal tract (digestive system) is commonly known as gastrointestinal (GI) bleeding. Gastrointestinal bleeding is one of the most common complain that warrant consultation with gastroenterologist (GI specialist). GI bleeding can be categorized into upper gastrointestinal bleeding and lower gastrointestinal bleeding.
The most common presentation for upper gastrointestinal bleeding include
- Hematemesis (vomit blood, that can be bright red or brown coffee grounds)
- Melena (black tarry stool)
- Hematochezia (if massive upper gastrointestinal bleeding of 1000 ml) although hematochezia usually presentation of lower gastrointestinal bleeding (colon usually)
 Causes of Upper Gastrointestinal Bleeding
Causes of Upper Gastrointestinal Bleeding
Table of Contents
The most common cause of upper gastrointestinal bleeding is peptic ulcer disease. We will look at them briefly. Details on each disease will be covered in more detail in another section.
- Peptic ulcer disease account for more than 50% of upper gastrointestinal bleeding.
- Portal hypertension accounts for 10-20% of upper gastrointestinal bleeding. The most common bleeding source arise from esophageal varices in patient with cirrhosis due seen in chronic alcoholics and patient with chronic hepatitis. Esophageal varices is most common but gastric and duodenal varices or portal hypertensive gastropathy can also be the source.
- Mallory Weiss Tears: laceration of the gastroesophageal junction cause 5-10% of upper gastrointestinal bleeding. This condition is commonly seen in chronic alcoholics with retching.
- Gastritis, Esophagitis like GERD (gastroesophageal reflux disease), Duodenitis, Gastric cancer with ulcerating tumor, esophageal cancer with ulcerating tumor all can cause upper gastrointestinal bleeding.
- Vascular abnormalities like angiodysplasia can also rarely cause upper GI bleeding.
The most common cause of upper gastrointestinal bleeding is ulcer disease. Most upper gastrointestinal bleeding can present with hematemesis or melena. Massive and rapid transit from high volume upper gastrointestinal bleeding can also present with bright blood (hematochezia) in stool.
Causes of Lower Gastrointestinal Bleeding
Lower gastrointestinal bleeding is defined as bleeding below the ligament of treitz. That is from the last two third of the duodenum until the anus. However, 95% of the source come from colon. The most common presentation of lower gastrointestinal bleeding is hematochezia (bright red bleeding). However, bleeding from ascending colon cancer can also present with melena. Note that 10% of hematochezia can arise from upper gastrointestinal bleeding. The most common cause of lower gastrointestinal bleeding is diverticulosis which present as painless colorless bleeding. The complete cause of lower gastrointestinal bleeding are as follows:
- Diverticulosis accounts for 50% of lower gastrointestinal bleeding, usually seen in patient > 50 years old but are increasingly seen in younger patients
- Benign polyps and Colon cancer accounts for 7% of lower gastrointestinal bleeding
- Infectious colitis also causes lower gastrointestinal bleeding
- Angiodysplasia can occur in upper and lower gastrointestinal tract and hence can present with both melena and hematochezia.
- Anorectal diseases like hemorrhoids and fissures usually result in small amounts of bright red blood noted on toilet paper, streaking of the stool or dripping into the toilet bowl. Hemorrhoids can be responsible fro 10% of lower gastrointestinal bleedings.
- Ischemic colitis is commonly seen in older patients with lower gastrointestinal bleeding. Most of them have atherosclerotic disease. Most occur spontaneously due to transient episode of non-occlusive ischemia of the bowel. They usually present with hemaochezia but can be melena as well.
- Inflammatory bowel disease especially, ulcerative colitis often have diarrhea with variable amount of hematochezia. Symptoms of tenesmus, abdominal pain and sometimes fever may be present.

Clinical Presentations of Gastrointestinal Bleeding
Most patient present with orthostasis which means more than 10 point rise in pulse when going from supine to standing of sitting. Another definition will be SBP (systolic blood pressure) drop of > 20 points when sitting up.
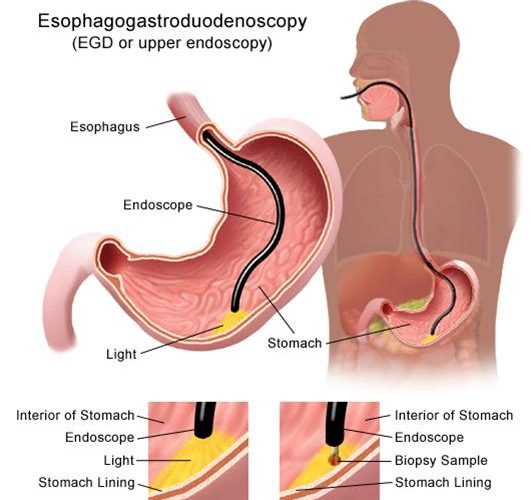
Management and Diagnosis of Gastrointestinal Bleeding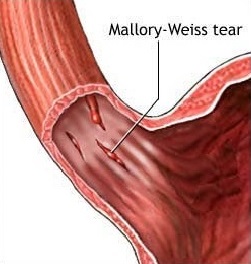
The most important thing that a doctor will do when you have GI bleeding is to assess your vital signs. You will be given IV fluids if you present unstable vital signs such as low blood pressure. Once your doctor is sure that you are getting ample fluids to maintain your blood pressure, they will begin their diagnostic process of finding the causing of bleeding.