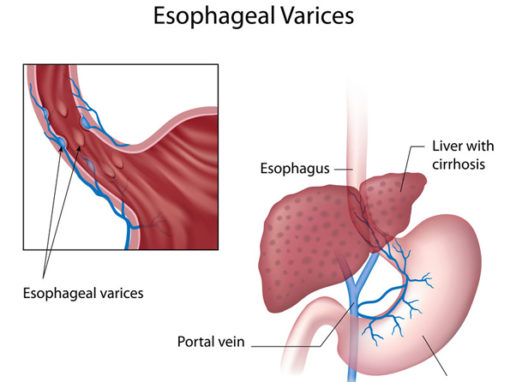
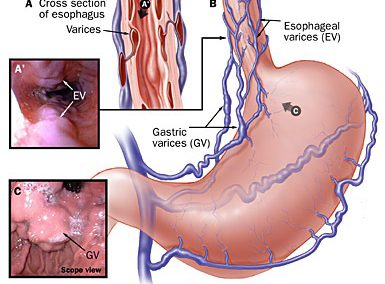
 Varices are dilated tortuous mucosa or submucosa veins that most commonly develop in the lower esophagus and Proximal Stomach. It is very common in patients with cirrhosis. This is because blood flow to the liver is blocked by the scarring liver. The backup pressure, increases the pressure inside the portal vein (which carry blood from the intestines to the liver.
Varices are dilated tortuous mucosa or submucosa veins that most commonly develop in the lower esophagus and Proximal Stomach. It is very common in patients with cirrhosis. This is because blood flow to the liver is blocked by the scarring liver. The backup pressure, increases the pressure inside the portal vein (which carry blood from the intestines to the liver.
When the blood pressure in the portal system is high (portal hypertension), the pressure back up and can cause dilation of veins. Portal hypertension causes an increase in the blood pressure in the veins in the lower esophagus and stomach. Because these veins are not meant to tolerate high pressure, they expand, dilate, resulting in varices. As the varices dilate and develop, they can overdistend and rupture, causing variceal bleed.
Etiology and Pathophysiology of Esophageal varices:
Table of Contents
Esophageal varices (EV) usually arise secondary to portal hypertension due to pathologies like cirrhosis or hepatocellular carcinoma (HCC).
Portal hypertension from liver cirrhosis (60% of have EVs) or HCC. Distal esophageal vein usually drain into the portal vein via the left gastric vein, but in portal hypertension, the left gastric vein back up into the esophagus vein, resulting in dilation (varices).
Risk factors include all causes of liver cirrhosis: Alcohol (most common), Wilson disease, Hemochromatosis, α1-Antitrypsin deficiency, Chronic Hepatitis (viral), Schistosomiasis, Sarcoidosis are all risk factors that can lead to post cirrhosis portal hypertension, eventually causing esophageal varices.
Symptoms and Clinical Presentation:
Esophageal varices are usually asymptomatic. It is estimated that 15% of patients who bleed from varices will die, emphasizing the need to prevent so. Varices do not cause symptoms until they rupture, causing massive painless bleeding, presenting as hematemesis, black stools, lightheadedness or loss of consciousness.
Have risk of rupture of the esophageal vein and present with painless hematemesis, dark stools, and lightheadedness. In addition to bleeding, all the symptoms of liver cirrhosis including portal hypertension complications such as ascites, hepatic encephalopathy, splenomegaly, gynecomastia, pedal edema, coagulopathy can also be present.
Complications of esophageal varices:
Esophageal Varices rupture: Most common cause of death in patient with cirrhosis (50%) (which causes the portal hypertension). A ruptured vein can cause potentially fatal hemorrhage
 Diagnosis of Esophageal Varices:
Diagnosis of Esophageal Varices:
Because of the serious consequences of bleeding, and because treatment can reduce this risk, experts recommend that all people with cirrhosis undergo testing to determine if varices are present. Patient with cirrhosis are recommended for testing to rule out varices before they bleed.
Patient under upper endoscopy will be managed depending on the present of varices: If no varices present, patient would need upper endoscopy every 2-3 years. If positive for varices, they need to followup for a recheck 1-2 years for possible enlargement. Medication may be commenced depending on the risk of bleeding.
Treatment and Management with varices without Bleeding
- Prevent bleeding
- Beta blockers is tolerated
- Avoid risk factors: alcohol, do weight loss which remove fat from liver and reduce injury
- Band Ligation (done during upper endoscopy)
- Placement of rubber bands around varices to prevent them from bleeding
- Upper endoscopy 2 weeks later to determine if additional bands are needed
- PPI (BID) to increase speed of healing of erosion/ulcers that develop when the bands fall off of the shrinking varix.
- Band ligation can be used (no bleed, bleed before, or if cannot tolerate propranolol)
Treatment and Management with Varcies and Bleeding
- Hemodynamic resuscitation
- Vitals (Blood pressure, Heart rate etc); CBC; PT/INR – Fluid replacement and Transfusion if needed (80% of GI bleed stop spontaneously if fluid resuscitation is adequate.
- Transfusion:
- pRBC (packed red blood cell) if Hemoglobin (Hb) < 10 for old patient; 7 for young patient.
- Platelets if bleed and platelet < 50,000. (If no bleeding, No platelet transfuse unless < 10-20k)
- FFP (free frozen plasma) if PT/INR elevated;
- Octreotide for variceal bleeding
- Prevention and treatment of complications of bleeding
- Antibiotics (Rocephin, Ciprofloxacin) and PPI for upper GI bleeding
- Aspiration Pneumonia, Sepsis: antibiotics may help
- Acute on Chronic liver failure
- Hepatic encephalopathy:
- Lactulose is an important treatment for patient with cirrhosis. Be sure to check potassium which may be low from vomiting.
- Hypokalemia may be a particular problem because it can promote the development of hepatic encephalopathy via increased renal ammonia production.
- Metabolic alkalosis, if hypokalemia induced by diuretics or vomiting, may also contribute by promoting the movement of ammonia across the blood-brain barrier.
- Thiamine replacement if patient still alcoholic on presentation.
- Renal failure (Acute tubular necrosis or Hepatorenal syndrome) – fluid resuscitation is important to prevent this complication
- Upper Endoscopy Aided Therapy
- Banding is more effective than sclerotherapy due to risk of stricture as side effect after sclerotherapy.
- No bleed post resuscitation – Initiate prophylaxis propranolol (band ligate 1-2 week later)
- Continued bleeding are treated with balloon tamponade followed by TIPS/Shunts (TIPS worsen hepatic encephalopathy)
- Re-bleeding varices after banding are treated with upper endoscopy therapy but if rebleed again followed by TIPS/Shunts.