Colorectal Carcinoma arising from colonic or rectal mucosa (peak incidence 60-70 years old). They are usually seen in older patients or young patient that usually have ulcerative colitis, chron’s or genetic predisposition phenotype like Familial Polyposis Syndromes (FAP) and Lynch syndrome (HNPCC).
Causes and Risk factors for Colorectal Cancer: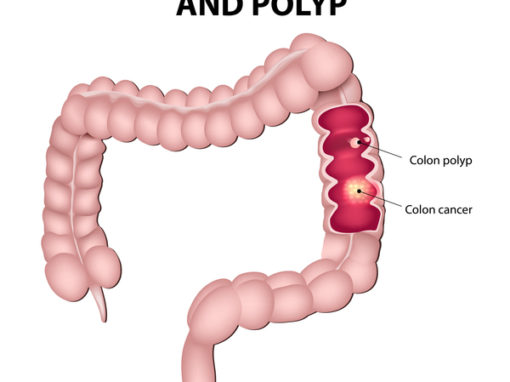
Table of Contents
The most common cause of colorectal cancer is due to the Adenoma-carcinoma sequence (APC, KRAS, P53 mutation) in 90%. The second most important molecular pathway to cause Colorectal cancer is MSI mutation (10%) which may or may not involve polyps.
Risk factors for develop colorectal cancer include: inflammatory bowel disease (IBD), smoking, low fiber high animal fat diet, obesity ad sedentary lifestyle.
Other association: Endocarditis with (Streptococcus bovis and Clostridium speticum) – hence any patient with endocarditis of these organism need colonoscopy to rule out intestinal malignancy.
Symptoms and Clinical Presentation
Colorectal cancer are usually asymptomatic until the tumor grows bigger to cause symptoms. Since most lesion begin with polyps, it is important to screen for polyps and remove them if found.
Right sided lesion present with fatigue, weakness and Fe deficiency due to blood loss (melena) from ulceration of tumor that’s bulky and bleed easily. Fe2+ Deficiency anemia found in elderly is GI Malignancy unless proven otherwise.
Left sided lesion present with altered bowel habits (obstruction) and bright red bleeding (hematochezia) that sometimes have pencil stools.
- Adenoma-Carcinoma Sequence
- Arise from APC/β-catenin: KRAS, P53/DCC mutation sequence
- Location is left sided (rectalsigmoid or distal colon), left lower quad (LLQ) pain
- Tumor present as Napkin-Ring Constriction Polyp type.(usually forms adenomaous polyps first)
- Cause obstruction of bowel (mainly), can also cause bright bleeding.
- Genetic predisposition: Germline APC mutation( lead to FAPs/Gardner/Turcot syndrome)
- MSI (microsatellite instability) Mismatch Repair Gene mutation Pathway.
- Arise from DNA mismatch repair gene mutations (MSH2, MSH6, MSL1, PMS etc)
- Location is right sided (Ascending/Proximal colon),right lower quad vague pain
- Tumor present as Exophytic mass Polyp type (may or may not form adenomatous polyps.)
- Cause Bleeding, hence Fe2+ deficiency anemia
- Genetic predisposition: Germline MSH2, MSL1 germline mutation (HNPCC=Lynch syndrome)
- Increase risk of other cancers: colorectal cancer, ovarian cancer, endometrial cancer, stomach, biliary tract, even small intestine, pancreas
- Carcinoma occurs denovo, not from adenomatous polyp at a very young age.
Morphology of Colon Carcinoma
- Usually solitary unless Genetically predisposed say FAPs
- Multiple cancers (ulcerative colitis, Polyposis syndromes, HNPCC)
- Neoplastic glands invading submucosa and beyond à regional LN (lymph node), Liver, Lung, Bones
- 10-15% may produce extensive mucin
Diagnosis of colorectal cancer
- Screening Guidelines:
- For No Genetic Risk Patient ≥ 50 years old.
- Colonoscopy every 10 years* best method.
- Fecal occult blood test yearly and if positive, you will need a colonoscopy (False Negative if Vitamin C consumed, False Positive if NSAID is being used.)
- Flexible Sigmoidoscopy or double contrast Barium every 5 years
- If dysplastic polyps found previous
- need Colonoscoy screening every 3-5 years
- If self had colon cancer
- 1 year post resection, then at 3 year, followed by every 5 year
- If Single FHx of cancer/polyps
- 10 yr before family has colon cancer /polyp OR 40 year old screen (whichever comes first)
- Need to repeat Colonoscopy every 3-5 years
- HNPCC (Lynch Syndrome) – MSI mutation (syndrome defined by 3 Family member in at least 2 generation have colon cancer
- Start at 25 years old (Colonoscopy every 1-2 years)
- High incidence of Ovarian and Endometrial cancer
- FAPS (Familiar Adenomatous Polyposis Syndrome)
- Start at 12 years old (Flexi sigmoidoscopy every 1-2 years)
- Polyps as early as 25 years old and 100% penetrance – colon cancer by 50 yr.
- If polyps positive (total colectomy) must be done and connect the terminal ileum to form new rectum.
- FAP variants (no screening recommendation yet)
- Gardner syndrome: Colon cancer associated with soft tissue tumors (Lipoma, Osteoma, Fibromsarcoma) – Osteoma especially at the Mandible – do colonoscopy if see any of the associated soft tissue tumor. Some recommend screen like FAP.
- Turcot syndrome: Colon cancer associated with CNS malignancy (GBM, Medulloblastoma)
- Harmatomatous Polyposis Syndrome (no recommendation yet)
- Juvenile Polyposis Syndrome (10% risk of colon cancer unlike FAPS) – only a few dozen unlike FAP thousands. Non-adenoma (Harmatoma) low risk cancer
- Cowden syndrome – rectal bleeding as a child (also harmatoma) only sligh risk than geneal population
- Dannayan-Ruvacalba-Riley syndrome
- Peutz-Jegher Polyps Syndrome
- For Patient with IBD
- Especially Ulcerative Colitis Diagnosed for 8-10 years, you need to screen with colonscopy every 1-2 years for colorectal cancer.
- For No Genetic Risk Patient ≥ 50 years old.
Diagnosis of Colon Cancer
- Colonoscopy (only 60% of colon cancer caught with sigmoidoscopy)
Post treatment Labs
- CEA useful to follow therapeutic response and detect recurrence, not good for screening.
- Also done before treatment to compare
Treatment of colon cancer
- Depend on stage and extend of spread.
- Metastatic Liver disease (One lesion) can be resected surgically, if > 1 lesion = chemotherapy.
- Localized (Mucosa, submucosa, muscularis mucosae) – can be resected for cure
- Penetrated the serosa or surrounding tissue and LN – Chemotherapy
- 5FU + Leucovirin
- Xeloda = Capecitabine = 5FU prodrug; Leucovirin = folinic acid
- New drugs – Avastin (Bevacizumab) which is a VEGF inhibitor that block vessel growth to supply the growing tumor.