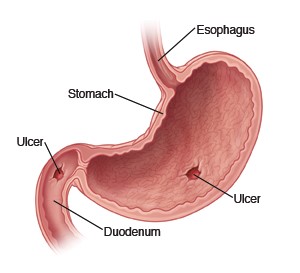
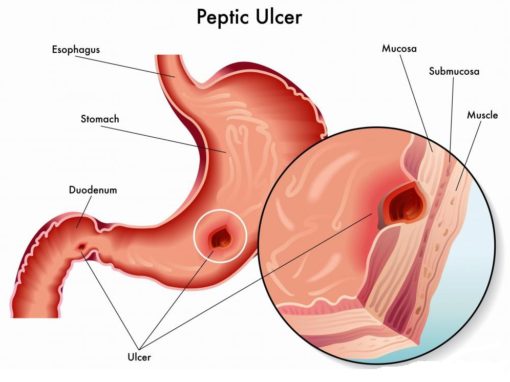
 This term refers to both gastric and duodenal ulcer disease. Peptic ulcer disease (PUD) is characterized by a defect in the gastric or duodenal mucosa that extends through the muscularis mucosa into the deeper layers of the wall. In addition to acid vs defense imbalance, there is mucosal damage by H. pylori (VacA, Urease, Protease, phospholipase) products or other potential non acid injuries. There is usually a mixture of acute and chronic inflammation
This term refers to both gastric and duodenal ulcer disease. Peptic ulcer disease (PUD) is characterized by a defect in the gastric or duodenal mucosa that extends through the muscularis mucosa into the deeper layers of the wall. In addition to acid vs defense imbalance, there is mucosal damage by H. pylori (VacA, Urease, Protease, phospholipase) products or other potential non acid injuries. There is usually a mixture of acute and chronic inflammation
Etiology and Association:
Table of Contents
- H.pylori infection (75% gastric, 90% Duodenal) is the most common cause.
- Non-H.pylori caused peptic ulcer disease are usually due to NSAIDS (most common), gastric cancer, Chron’s disease, Gastrinoma (ZES).
- Other acute stress and trauma like burns, head trauma, intubation can also cause acute stress ulcers.
- Note that NSAIDs inhibit the production of mucus barrier because prostaglandin produce the mucus. This is the most common cause of non- H.pylori cause PUD.
- Smoking and Alcohol delay healing but does not cause ulcers – simply worse and prevent healing.
Symptoms and Clinical Presentation
- Epigastric pain (that worsen at night, dull and sore and gnawing), hematemesis, non-tender unless perforation is present.
- Post feeding symptoms: (worsen for gastric ulcer), (better for 1-3 hours for duodenal ulcer)
- Weight loss from decreased PO due to pain is common, hence more common in gastric ulcer instead of duodenal, however, it is impossible to differentiate ulcer, gastritis, non-ulcer dyspepsia without upper endoscopy.
- Perforation can be a severe complication: Symptoms of peritonitis include guarding and lying still with refusal to move.
 Diagnosis of Peptic ulcer disease
Diagnosis of Peptic ulcer disease
You can’t tell the difference between Duodenal and Gastric ulcer just based on symptom from eating, because its only suggestive and hence need upper endoscopy to tell difference. The threshold to scope is low (45 years old with epigastric pain) because need to exclude cancer since cancer can be a cause (4%) of ulcers.
The most accurate diagnostic test is upper endoscopy (if positive, there is a need to biopsy the ulcer for ruling out cancer). Biopsy is important to distinguish type of ulcer and also rule out ulcerating cancer.
- Test for Helicobacter pylori – this is important because the ulcer will recur or non-responsive to treatment with PPI only. This is because they need to be treated with triple therapy.
- Barium study – can detect ulcer (not cancer or H.pylori) hence not commonly done.
- Biopsy Pathology: The peptic ulcers usually have have round to oval, punched out with relatively straight walls hence raised and sharp margins. Smooth and clean base of ulcer, ulcers are usually solitary (unlike acute ulcer multiple). Radiating surrounding mucosal folds are usually present.
- Active ulcer has 4 zones:
- Necrotic fibrinoid debris
- Non-specific inflammatory infiltrate (mainly PMN)
- Granulation tissue (fibrotic healing)
- Fibrosis and collagenous scar (fibrotically healed)
Complications of Peptic Ulcers.
- Hemorrhage (most common)
- Perforation: potential perforation that lead to bleeding and peritonitis (anterior perforation) and pancreatitis (posterior perforation) can present with sepsis and would see air under diaphragm.
- Fe2+ Deficiency anemia (due to chronic loss of blood)
- Pyloric obstruction: is the narrowing of pyloric canal by scarring and swelling of gastric antrum and duodenum due to peptic ulcers. Patient often present with severe vomiting without bile
- Cancer of stomach (need to rule out especially if H.pylori caused), rare and almost never in duodenum. In stomach usually adenocarcinoma – intestinal type(note goes to supraclavicular node Metastasis)
Treatment and Management
- Ulcer without H.pylori/Cancer – PPI is usually sufficient treatment in 90% of the case.
- Ulcer with H.pylori – triple therapy (2 weeks) – see below if no resolve. PPI treatment will recur if no antibiotics are used. Standard of Care: Triple Therapy (CAP) if fail, replace with antibiotic Flagyl, Tetracycline.
- Selection of Triple Therapy Regimen:
- PPI + Clarthromycin + either (Amoxicillin if no Penicillin allergy) or Flagyl (if Penicillin allergy)
- Check with upper endoscopy for resolution of Ulcer* (see if ulcer become cancer via biopsy during upper endoscopy) 1-2 months post therapy
- Stool Antigen or Urea test to see if failed ulcer treatment is from persistent H. pylori
- Change medication antibiotics and add bismuth if persistent H. pylori infection.
- Medical treatment failure usually from
- Nonadherence to meds, alochol, Smoke, NSAIDs
- Surgery indicated if complication like (hemorrhage, perforation, gastric outlet obstruction) develop
- Perforated Ulcer: IVF (IV fluid), PPI, Antibiotics (broad spectrum especially, gram negative) – even if suspected, need to do all 3 as well