Diabetic gastroparesis defines as lack of motility of the stomach due to lack of responsive whether sensory or effector functions of the nervous system innervating the stomach.
Normal gastrointestinal motor function involves a complex coordination and series of events that involve the autonomic nervous system (sympathetic nervous system (SNS) and parasympathetic nervous systems), neurons and pacemaker cells (also called interstitial cells of Cajal) that are found within the stomach and even intestines, smooth muscle cells of the gastrointestinal tract.
Any deviation from the series of ordered and coordinated process can result in delay in emptying of the stomach.
Causes of Diabetic Gastroparesis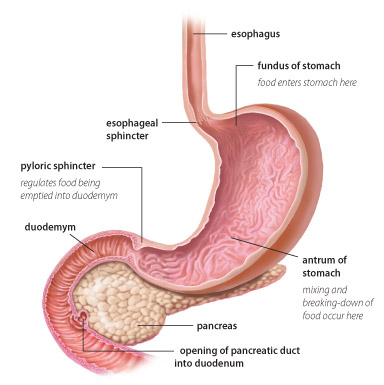
Table of Contents
This is due to long standing diabetes mellitus especially with poor sugar control for more than 10 years. The lack of sugar control lead to neuropathy and hence the stomach and intestines cannot sense stretch from food. (nerve supply to the bowel is impaired)
As mentioned, usually stretch and distention of intestine and stomach leading to motility. Gastroparesis lead to autonomic neuropathy leading to dismotility from inability to sense stretch hence no normal motility.
Vascular damage to the nerves of digestive tract affect a person’s ability to detect the stretching and distension of the stomach on food arrival.
Cause of Diabetic Gastroparesis
Cause of gastroparesis can be idiopathic. However, the most common cause of gastroparesis is poor diabetic sugar control for more than 10 years are usually a risk factor for developing gastroparesis.
Post surgery especially from nissen fundoplication, Other risk factors include infiltrative disease (amyloidosis, scleroderma), multiple sclerosis (MS) and medication: TCA, calcium channel blockers (CCB), dopamine agonist, muscarinic antagonist, Octreotide, GLP-1 agonist.
Clinical Presentation of Diabetic Gastroparesis
Bloating, abdominal distention, constipation and diarrhea are common symptoms. Nausea, vomiting, early satiety can also be present. On physical exam, retained material > 3 hours in stomach will generate a splash sound – indicating filled with fluid.
Diagnosis
Gastroparesis should be suspect if a patients present with nausea, vomiting, postprandial fullness and early satiety. In addition, abdominal pain, or bloating can also be commonly seen. Imaging are usually used to rule out mechanical obstruction with CT or MRI or upper endoscopy. The presence of delayed gastric emptying on scintigraphy establishes the diagnosis of gastroparesis. Clinically diagnosis occurs usually but can use (nuclear gastric emptying study scintigraphy which is considered the most accurate study but rarely needed)
Treatment and Management:
Initial management of gastroparesis consist of dietary modification, optimization of glycemic control. If symptoms are persistent, medical treatment can be commenced.
You can commence medication with prokinetics like metoclopramide in all (mild, moderate, severe gastroparesis) and antiemetics like benadryl.
Other medications include motilin domperidone, erythromycin.
In patients with refractory symptoms despite dietary modification, prokinetics, and antiemetics, more invasive approach may be considered. Placement of a jejunostomy and venting gastrostomy tube for enteral nutrition and decompression, respectively.
Parenteral nutrition only in those who are not able tolerate enteral nutrition despite concomitant medication therapy.
Gastric electrical stimulation only in patients with gastroparesis with intractable nausea and vomiting despite medical therapy for at least one year.