 Barrett’s Esophagus is a complication of GERD. It has to do with metaplasia of lower esophagus mucosa from stratified squamous epithelium that normally lines the distal esophagus to non-ciliated columnar epithelium (glandular type: protective type of epithelial cell) with goblet cells (seen in 10% of GERD patients). Barrett esophagus is a precancerous lesion that can lead to adenocarcinoma of the esophagus and therefore most be monitored and prevented in patient with chronic acid reflux disease.
Barrett’s Esophagus is a complication of GERD. It has to do with metaplasia of lower esophagus mucosa from stratified squamous epithelium that normally lines the distal esophagus to non-ciliated columnar epithelium (glandular type: protective type of epithelial cell) with goblet cells (seen in 10% of GERD patients). Barrett esophagus is a precancerous lesion that can lead to adenocarcinoma of the esophagus and therefore most be monitored and prevented in patient with chronic acid reflux disease.
Etiology and risk factors for barrett esophagus:
Table of Contents
The cause of barrett esophagus, as mentioned is due to long standing lower esophageal acid irritation (GERD) leading to metaplasia as an adaptive approach to protect the mucosa of lower esopagus from acid damage. This typically occur in individual with 5 years of GERD.
Other causes or barrett esophagus not due to reflux disease include oral bisphosphonate.
Pathophysiology:
- 5 years GERD cause (columnar metaplasia) → dysplasia (↓ grade) dysplasia (↑ grade) → adenocarcinoma of esophagus
Symptoms and Clinical Presentation:
- Patient’s with barrett esophagus have similar signs and symptoms of GERD – No clear guideline after how long need upper endoscopy (but if patient have alarm symptoms, they need upper endoscopy and may at that point diagnose Barrett Esophagus.)
- GERD associated with long-segment Barrett’s esophagus frequently is complicated by esophageal ulceration (odynophagia), stricture (dysphagia), and hemorrhage (upper GI bleeding).
- Barrett’s usually do not have dysphagia unless concomitant esophageal/peptic stricture occurs due to long standing GERD.
Diagnosis:
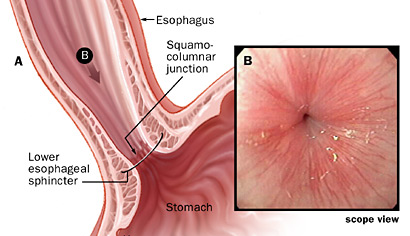
- Upper endoscopy is the most accurate approach to diagnose barrett esophagus with biopsy of the cells at the distal esophagus. Biopsy of area that look like a salmon pink patch (corressponding to the metaplasia area)
- Barium swallow is typically normal
Complications
- May progress to dysplasia → adenocarcinoma of esophagus
Treatment and management:
- Once diagnosed with Barrett Esophagus – patient needs the following medications.
- All patient with diagnosed barrett’s esophagus should be on (proton pump inhibitors) PPI.
- Upper Endoscopy for every 2-3 years to see if there is dysplasia (after metaplasia) or cancer development:
- Low grade dysplasia – need every 3 to 6 months upper endoscopy to follow up (resolve or progress)
- High grade dysplasia – Endoscopy Ablation with distal esophagectomy or endoscopic mucosal resection, radiofrequency ablation.